Antibiotics
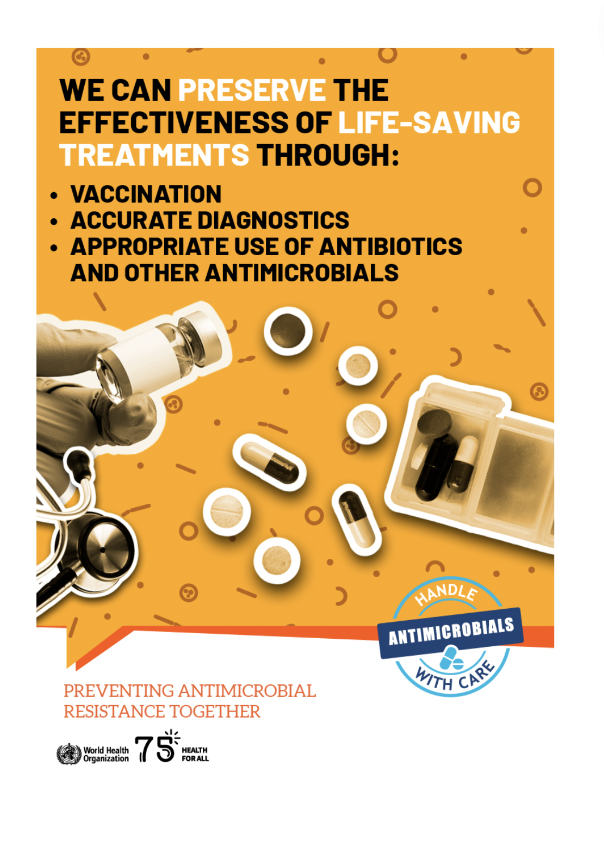
The antibiotic amoxicillin in child-friendly form (dispersible tablets) is the first-line recommended treatment for childhood pneumonia but is often unavailable in low-resource settings. A recent study showed that less than one-half of public health facilities in Tanzania stocked amoxicillin dispersible tablets, and nearly two-thirds had experienced stock-outs in the previous 90 days. While it is difficult to determine antibiotic coverage for children with pneumonia as no reliable measurement indicator exists, some studies report low coverage while others document overuse. Access to antibiotics for pneumonia must be considered in the context antimicrobial resistance. A recent study in Bangladesh concluded that the “pandemic of antibiotic resistance” is shortening the lives of children with pneumonia, and new approaches to prevent and treat these infections are “desperately needed.” The key challenge is to reduce the overuse of antibiotics for the treatment of pneumonia and, at the same time, tackle the access treatment gaps, especially among children, without triggering further waves of antimicrobial resistance.
Read more in the Every Breath Counts Access to Antibiotics Statement.
Medical oxygen
Oxygen is a life-saving treatment for many patients with pneumonia who are also hypoxemic – having low oxygen saturation in their blood. If untreated, they are at high risk of death. Studies have revealed that many countries faced a critical shortage of medical oxygen prior to COVID-19, with as many as one in five children with hypoxemia missing out. With the oxygen supplies more than 100 countries received during the pandemic, now is the time to ensure that every country has the medical oxygen needed to treat every patient, and the clinicians, engineers, and technicians needed to install, operate, and maintain the equipment. The new Global Oxygen Alliance (GO2AL), co-chaired by Unitaid, the Global Fund to fight AIDS, Tuberculosis and Malaria, the Africa CDC, and PAHO, and involving 20 leading global health agencies will continue to help countries increase access to medical oxygen to save lives now and prepare for the next pandemic.
Read more about how Every Breath Counts has been supporting access to medical oxygen prior to, during, and after the COVID-19 pandemic, and view the deck on oxygen and UHC here.
Universal Health Coverage (UHC)
For the more than 400 million adults and children who get sick with pneumonia each year, the costs of treatment can be crippling. In settings where there is no universal health coverage (UHC) and individuals and families are forced to pay out-of-pocket for healthcare, the costs can be catastrophic – plunging people into poverty, or further into poverty. In these countries, reducing pneumonia deaths will depend on how effectively governments can reduce the costs of treatment by ensuring pneumonia is part of national UHC schemes. In an acknowledgement of the importance of pneumonia, the UHC Service Coverage Index includes an indicator on pneumonia care seeking and the latest WHO and World Bank UHC Monitoring Report reveals how dismally many countries are performing on this indicator. Only health systems where more than 90% of children with pneumonia symptoms are taken for care have truly achieved UHC.
Read the Every Breath Counts UHC Statement here, learn more about the Every Breath Counts UHC campaign, You Paid WHAT? The Crippling Costs of Pneumonia Treatment, and share your story here.